Oral Chronic Graft-Versus-Host Disease
Chronic graft-versus-host disease (cGVHD) is a frequent and serious complication following allogeneic hematopoietic stem cell transplantation (HSCT), also known as “bone marrow transplantation” (BMT; for explanation of these terms see sidebar). It usually develops within the first 6 to 24 months following HSCT.
|
Allogeneic Bone Marrow Transplantation
Hematopoietic stem cell transplantation (HSCT) is a medical procedure that is used to replace the blood forming elements of a patient who develops a malignancy within the blood forming system. In preparation for this procedure the patient is treated with high doses of chemotherapy, often combined with total body irradiation to destroy their existing blood forming cells. Increasingly, reduced intensity conditioning regimens are being used which take advantage of the "graft-versus-leukemia" effect while avoiding much of the transplant-associated toxicity of traditional "fully myeloablative" regimens. Donor stem cells come from HLA matched related (e.g. siblings) or unrelated donors (identified through international registries).
|
The skin, liver, mouth and eyes are the most commonly affected parts of the body, and can be associated with significant quality of life deficits. Some degree of cGVHD is likely a good thing as it is a sign of successful acceptance of the graft and may help keep the underlying disease in long-term remission due to the so called “graft-versus-leukemia effect”. Oral cGVHD is very common and in some cases, the mouth may be the only area affected. The symptoms associated with oral cGVHD include mouth pain, sensitivity to normally tolerated foods and drinks, reduced mouth opening, and dry mouth.
What Causes Oral Chronic GVHD?
The engrafted donor immune cells recognize parts of the patient’s body as “foreign” and mount an immune attack. The risk of developing cGVHD is greatly dependent on how well “matched” the donor was to the recipient. While oral cGVHD is seen to a greater degree in poorly matched transplants, it can still develop even in ideally matched situations.
How Does Oral Chronic GVHD Appear in the Mouth?
Several forms of oral cGVHD are recognized, all of which can be present at the same time. The most common is the reticular form (Panel A) that looks like lacy white lines – usually on the inner cheek or the sides or top of the tongue. These lesions are often not painful and may be present for a long time before being noticed. A second form is the erosive form. These look like raw, scraped, red areas that are often painful and sore, particularly when contacted by food. Faint subtle white reticulations may be seen at the edges of the red areas. A third form is the ulcerative form (Panel B). This form appears smooth and yellow and is generally very painful. These lesions may look like canker sores and can be quite large.
 
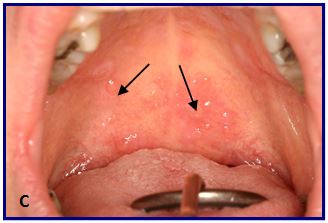 Oral cGVHD may also affect the salivary glands, resulting in dry mouth and/or the development of small blisters (superficial mucoceles) on the inside of the lips and the palate (Panel C). Mucoceles can come and go with meals and are typically more of a nuisance than actually painful. Oral cGVHD may also affect the salivary glands, resulting in dry mouth and/or the development of small blisters (superficial mucoceles) on the inside of the lips and the palate (Panel C). Mucoceles can come and go with meals and are typically more of a nuisance than actually painful.
 Patients with dry mouth may have difficulty chewing and swallowing foods, may notice changes in taste, and are at increased risk for developing dental caries, especially along the gum line and interproximally, between the teeth (Panel D). Finally, in patients who develop thickening and hardening of the skin due to cGVHD (the sclerotic form of cutaneous cGVHD), the same process may affect the skin of the face and neck, and in some cases, even the soft tissues inside of the mouth. When this happens the mouth may feel “tight” and it may be difficult and even painful to open the mouth for normal daily functions. Patients with dry mouth may have difficulty chewing and swallowing foods, may notice changes in taste, and are at increased risk for developing dental caries, especially along the gum line and interproximally, between the teeth (Panel D). Finally, in patients who develop thickening and hardening of the skin due to cGVHD (the sclerotic form of cutaneous cGVHD), the same process may affect the skin of the face and neck, and in some cases, even the soft tissues inside of the mouth. When this happens the mouth may feel “tight” and it may be difficult and even painful to open the mouth for normal daily functions.
QUESTIONS AND ANSWERS ABOUT ORAL CHRONIC GRAFT-VERSUS-HOST DISEASE
Q: How do I know if I have oral chronic GVHD?
A: Usually your oncologist or an experienced oral medicine specialist can diagnose oral cGVHD by correlating the clinical findings and symptoms with the medical history. In some circumstances however, a biopsy may be necessary.
Q: What should I expect once I have been diagnosed with oral chronic GVHD?
A: Oral cGVHD severity is variable and symptoms tend to come and go. Some days it will feel better, and other days it may feel worse. It tends to get worse if your body is stressed, both physically (such as having a cold) and emotionally. It is usually best to avoid spicy and acidic foods, as they will generally aggravate your mouth. However there are no specific foods that actually make the condition get worse. Oral cGVHD can persist for many years, although it tends to burn out after the first couple of years. If you have a dry mouth, this may further worsen the condition and put you at high risk for developing dental decay.
Q: Is oral chronic GVHD contagious?
A: No. Oral cGVHD is not an infection and you cannot spread it to family members and friends.
Q: How do I treat my oral chronic GVHD mucosal lesions?
A: There is no cure for oral cGVHD. However, your doctor can prescribe therapies to alleviate pain and reduce inflammation. For acute pain relief, your doctor may prescribe a topical anesthetic such as viscous lidocaine to be applied to the lesions. To reduce the inflammation, your doctor will usually prescribe an anti-inflammatory agent, such as a steroid, to be applied topically. A non-steroidal anti-inflammatory ointment called Protopic may also be prescribed, in particular for treating the outer part of the lips.
If the lesions are extensive or difficult to reach, the most effective approach is to rinse with a steroid solution (dexamethasone or another potent steroid) for 5 minutes prior to spitting out, 2-4 times each day. High potency corticosteroid gels such as fluocinonide or clobetasol, can be used to treat localized problem areas. After cleaning your mouth, dry the area with some cotton gauze, place a small amount of gel on a clean finger, and dab it onto the painful areas. To maximize the effectiveness of any topical steroid, you should not eat or drink for 10-15 minutes after application. There is no harm in swallowing the small amount of residual steroid that may wash away from the lesion. When using a steroid preparation, your risk of developing an oral yeast infection is increased. Thus, your doctor may prescribe an antifungal medication to either prevent, or if necessary, treat the yeast infection.
After the symptoms have been brought under control, it is a good idea to let the mouth rest rather than use the steroid continuously when not experiencing pain. When a flare-up occurs, the prescribed medications can be used as previously instructed. However, if improvement is not noted within 1-2 weeks, you should see your doctor.
Q: What can I do to treat my mouth dryness?
A: If your mouth feels dry, avoid caffeinated and alcoholic beverages and drink plenty of water throughout the day. There are specific “dry mouth” products that are available over the counter such as the Biotene and Oasis line of products that may help relieve the symptoms to some degree. In addition, medications such as Salagen and Evoxac may be prescribed to actually help stimulate the salivary glands to produce more saliva, and these can be extremely effective for some patients. The daily application of both a prescription strength home fluoride gel such as Prevident 5000 as well as a remineralizing agent such as GC MI Paste, are essential to prevent dental caries. Your dentist may also recommend more frequent check-ups. For more information on this topic see the separate sheet on xerostomia.
Q: Is oral chronic GVHD a risk factor for oral cancer?
A: Patients with cGVHD are at a significantly increased risk for developing oral cancer and should undergo an oral cancer screening at least once a year. Since oral cGVHD can look similar to early oral cancer, it is best to be seen by a specialist who is familiar with these conditions. Periodic biopsies of suspicious lesions may be necessary.
Recommended Links:
Prepared by N. Treister and the AAOM Web Writing Group
Updated 22 January 2015
The information contained in this monograph is for educational purposes only. This information is not a substitute for professional medical advice, diagnosis, or treatment. If you have or suspect you may have a health concern, consult your professional healthcare provider. Reliance on any information provided in this monograph is solely at your own risk. |


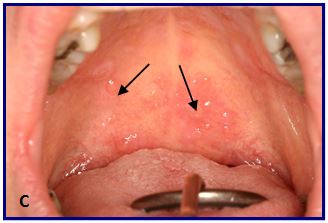 Oral cGVHD may also affect the salivary glands, resulting in dry mouth and/or the development of small blisters (superficial mucoceles) on the inside of the lips and the palate (Panel C). Mucoceles can come and go with meals and are typically more of a nuisance than actually painful.
Oral cGVHD may also affect the salivary glands, resulting in dry mouth and/or the development of small blisters (superficial mucoceles) on the inside of the lips and the palate (Panel C). Mucoceles can come and go with meals and are typically more of a nuisance than actually painful. Patients with dry mouth may have difficulty chewing and swallowing foods, may notice changes in taste, and are at increased risk for developing dental caries, especially along the gum line and interproximally, between the teeth (Panel D). Finally, in patients who develop thickening and hardening of the skin due to cGVHD (the sclerotic form of cutaneous cGVHD), the same process may affect the skin of the face and neck, and in some cases, even the soft tissues inside of the mouth. When this happens the mouth may feel “tight” and it may be difficult and even painful to open the mouth for normal daily functions.
Patients with dry mouth may have difficulty chewing and swallowing foods, may notice changes in taste, and are at increased risk for developing dental caries, especially along the gum line and interproximally, between the teeth (Panel D). Finally, in patients who develop thickening and hardening of the skin due to cGVHD (the sclerotic form of cutaneous cGVHD), the same process may affect the skin of the face and neck, and in some cases, even the soft tissues inside of the mouth. When this happens the mouth may feel “tight” and it may be difficult and even painful to open the mouth for normal daily functions.