|
Return to the Fall 2021 Newsletter News from SchoolsThe University of California San Francisco (UCSF)Alessandro Villa, DDS, PhD, MPH The Oral Medicine Program at UCSF is home to six residents supported by GME funding. Summer is an exciting time for our oral medicine residency as we recently welcomed two new residents. Dr. Anette Vistoso Monreal is a dental graduate from Chile. Before joining UCSF, she completed a Master Program in Orofacial Pain and Oral Medicine at the University of Southern California. Dr. Chitra Emperumal earned her BDS from India and pursed further training in Orofacial Pain at the University of Southern California. Drs. Monreal and Emperumal are looking forward to expanding their knowledge in oral medicine and exploring new research opportunities in the field of oral oncology. Our second-year resident Dr. Abrar Baksh completed a one-year fellowship at the University of Maryland. She is working on a project on oral manifestations of inflammatory bowel disorders in pediatric patients. Dr. Morooj Aljish (PGY-2) obtained her dental degree at the Imam Abdulrahman Bin Faisal University in Saudi Arabia and now exploring new therapeutic options for the treatments of oral leukoplakia. Dr. Abdulrahman Abdullatif is also a dental graduated from Saudi Arabia. Before joining the oral medicine team at UCSF, he earned his Master’s degree in 2016 from the University of Buffalo where he completed a thesis on MRONJ among oncology patients. Our chief resident, Dr. Zahra Alsafwani (PGY-3) joined us in 2019 after completing a one-year fellowship in medically compromised patients at the University of Pennsylvania. Dr. Alsafwani is currently conducting a research study on the use of telemedicine in oral medicine. In addition to training the next generation of educators, scientists and oral medicine clinicians, our program seeks to foster interdisciplinary collaborations and combat health disparities.
From left to right: Drs. Vistoso, Baksh, Alsafwani, Emperumal, and Aljish (Dr. Abdullatif is not in the photo) Brigham and Women's Hospital/Harvard School of MedicineAdvanced Graduate Education Program in Oral Medicine, Harvard School of Dental Medicine and Brigham and Women’s Hospital Outgoing/incoming residents: In June 2021, we held a virtual graduation ceremony for our senior residents. Dr. Shaiba Sandhu, chief resident 2020-2021, has graduated and now joined the Orofacial Pain residency program at the Massachusetts General Hospital. Dr. Rossella Intini completed her training and returned to Europe. She will begin her PhD study at the University of Valencia, Spain. By July 2021, we have welcomed our new residents. Dr. Petros Yoon left his position as the Medical Director of the Salud Family Health Center in Aurora, Colorado to join our certificate program. Dr. Lama Alabdulaaly graduated with DMSc in Oral and Maxillofacial Pathology at Harvard School of Dental Medicine and started her training in oral medicine with us. Lastly, Dr. Abdulrahman Nakshabandi, a native of Saudi Arabia, has joined us in the combined DMSc and certificate track. Welcome, all.
Virtual graduation ceremony Awards of any member of your Department/School:
University of Washington School of Dentistry
David Dean, DDS, MSD, DABOM, FDS RCSEd Outgoing/incoming residents:
Awards of any member of your Department/School:
Brief scientific information about discoveries and breakthroughs related to oral medicine or other disciplines: Dr. Trayvon Foy presented a virtual poster at UWSOD research day suggesting no correlation between length of the ossified portion of the stylohyoid ligament and head and neck symptoms consistent with Eagle’s syndrome (e.g., dizziness, ear pain) in a cohort of TMD and H/N pain patients. He was mentored to OM faculty Dr. Stuart Taylor. Legislative/policy updates of the AAOM or of other: From Dr. Kim Espinoza - For the field of special care dentistry, there is a resolution from ADA Council on Dental Education (CDEL) to the ADA Hose of Delegates, specifically Resolution 46, which urges SCDA (Special Care Dentistry Association) to "pursue an accreditation process and accreditation standards for advanced education in special needs dentistry by the Commission of Dental Accreditation.” On October 14, 2021, there will be a meeting with the Dental Education Reference Committee at the ADA Annual Session where ADA members can testify on this resolution. Case Western Reserve University, School of Dental Medicine in Cleveland, Ohio
Andres Pinto, DMD, MBA, MSCE Chair and Professor, Oral and Maxillofacial Medicine and Diagnostic Sciences, School of Dental Medicine Upcoming events:
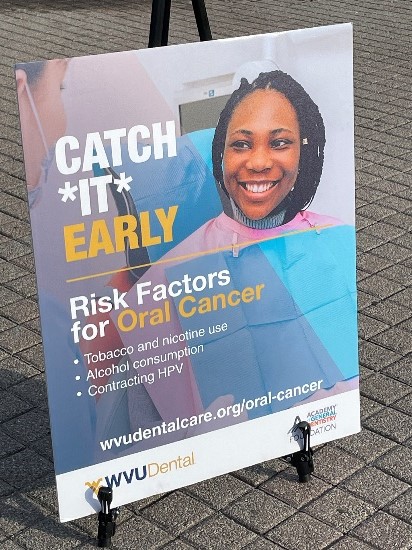
Outgoing/incoming residents: We currently have two oral medicine fellows starting July 2021 and one continuing MscD student. One MScD student successfully defended his research in July, and we graduated two OM fellows in December 2020. Awards of any member of your Department/School: Our department encompasses all diagnostic disciplines. Our oral and maxillofacial radiologist was inducted in the State of Ohio Radiology Safety Committee. Our oral and maxillofacial pathology faculty was awarded this fall seed grant funding to enhance his current genetic research. Dr. Milda Chmieliauskaite received continued FLRP federal support. She is engaged in several inter-institutional research projects. Dr. Pinto was named interim infection control officer for the Health Education Campus. Personal contributions on topics related to our discipline: Dr. Pinto was a guest speaker at the EAOM meeting in late September, 2021. He discussed opportunities for international OM collaboration in a panel with leaders of all OM global societies. He will also co-present a seminar on Practice Models of OM for the AAOM together with Dr. Michael Brennan on October 5, 2021 and gave invited talks to several international groups over the summer, including the Saudi Society of Oral Medicine. He will be a featured speaker for the International College of Dentists in December. Profile of your Department/School: Case Western Reserve School of Dental Medicine Department of Oral and Maxillofacial Medicine and Diagnostic Sciences Education: Fourteen DMD courses, six graduate core courses Training: Internship in OM, MScD in OM, fellowship in OM Internship in OMFR, MScD in OMFR School lead for VR / Hololense anatomy teaching Working on proposal to become a Center of Excellence in Orofacial Pain West Virginia University School of DentistryMore than 150 oral cancer screenings provided by dental school and WVU Dental clinics: event designed to promote oral cancer awareness and discuss risk factors.
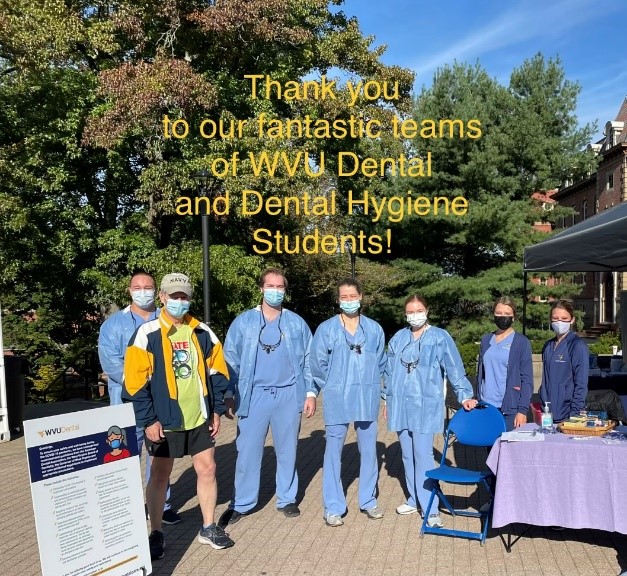
Information submitted by Elizabeth Southern Puette, MSDH, CTTS Organizers and providers at an oral cancer screening and awareness event at West Virginia University were eager to host an outreach project they believe could be lifesaving. “Oral cancer that is diagnosed early has better outcomes in terms of treatment, quality of life and life expectancy,” said Dr. Juan Bugueno, oral medicine expert and assistant professor at WVU School of Dentistry. As part of its mission to provide comprehensive oral healthcare and support overall patient wellness, the dental school, supported by the Academy of General Dentistry Foundation (AGDF), hosted “Catch It Early”, a free oral cancer screening and awareness initiative September 25, 2021. Adults 18 and older were invited to the downtown campus and WVU campus recreation for oral cavity screenings where dental and dental hygiene students checked for irregularities on all sides of the tongue and underneath. By feeling the tissues in the mouth and neck, the future providers tried to detect lumps or abnormalities. In five hours, 175 people received screenings. Patient Education The outreach event afforded dental school students the opportunity to share tobacco and nicotine cessation strategies, information about human papilloma virus and its connection to oropharyngeal oral cancer and suggestions on when patients should see a dentist, especially to detect lesions early. “While oropharyngeal cancer can be most prevalent in middle aged men and women, a younger population of men and women is not exempt from developing oral or oropharyngeal cancer,” said Elizabeth Southern Puette, assistant professor in the dental school’s department of dental hygiene. Patients were educated to look for symptoms like sores, lumps or even difficulty chewing. “Oral cancer is the appearance of lesions in any part of the mouth that need immediate attention and appropriate care. First, we want patients to avoid the development of oral cancer. Secondly, we want patients to be aware of suspicious lesions in the mouth,” Bugueno said. Volunteers also provided information about WVU Dental resources and clinical services that include but are not limited to teledentistry and specialty services such as a biopsy service, oral medicine clinic, oral and maxillofacial radiology, forensic dentistry and other oral diagnostic specialty services. Following Up Thanks to support from WV Mountains of Hope Cancer Coalition, participants received a self-oral cancer screening kit: a plastic mouth mirror, a flashlight, and self-oral screening instructions. Participants were taught how to conduct their own two-minutes self-screening at home and were encouraged to do so once a month in front of the bathroom mirror, right after they brushed their teeth. Packets also contained literature about oral cancer, early diagnosis and tips to reduce risk factors. Providers discussed personalized tobacco cessation information with patients, distributed 18 Nicorette samples and made referrals to the WV Tobacco Quitline. Of the 175 participants at the screening, 72 were recommended for dental hygiene services resulting in five appointments for dental prophylaxis appointments two days after the event. Another 28 participants were recommended for “further evaluation and treatment by a dentist”, and two patients were referred to the WVU Dental Diagnostic Sciences department for further review of a suspicious lesion. Continuing Education for Providers In addition to patient screenings, the dental school and WV Oral Health Program hosted a free continuing education webinar open to professionals in fields including dentistry, medicine, nursing, pharmacy and respiratory therapy. Continuing education presenters encouraged the use of evidence-based strategies in tobacco cessation counseling. Health professionals learned the importance of implementing routine screening strategies to identify oral cancer lesions early and next steps; including an overview of risk factors, referrals, biopsy services, and adjunctive aids to help identify suspicious lesions. Other objectives of the course included:
Volunteers Thank you to the s8tudent volunteers and patients who participated in the Oral Cancer: Catch It Early event. Faculty volunteers included specialist ranging from oral medicine, to pathology, to smoking cessation, to oral cancer related dental care. Additional faculty volunteers included Dr. Fotinos Panagakos, associate dean for research, Dr. Brian Whitaker, interim chair of the department of diagnostic sciences, and assistant professor Dr. Hiba Qari. Dental hygiene students served as site managers. Supporters of Oral Cancer: “Catch It Early” included:
Precautions during COVID Prior to any screenings, student volunteers were responsible for COVID pre-screenings. All volunteers passed a COVID screening upon arrival to the oral cancer screening sites that included questions about history, current symptoms and a temperature check. Participants were required to pass the COVID screening, as noted in promo and advertising leading up to the event. Distancing and masking protocols were in place. Hydrogen peroxide pre-rinses were used as an additional precaution.
|


 The Oral Medicine group at BWH led by Dr. Piam Vacharotayangul, Dr. Brittany Klein (PGY-2) and Dr. Nathaniel Treister were awarded a significant fund through the United Against Racism initiative from the Mass General Brigham system. Aimed to address disparities in access to our oral medicine specialty from the underserved population, the fund will be used to systemically generate awareness of our practice to the general public and professional communities in Boston and its vicinities. By connecting to and establish a clinic in the local community health centers, the oral medicine group at BWH will be providing care to the people directly in the community and reducing the burden of commuting and waiting time to see our specialists. The team will foster trust by promoting a continuous commitment of the specialists within the underrepresented community, by providing education and outreach into the community on a regular basis, by demonstrating the outcomes that can be achieved, and by facilitating the referral to or access to specialized care clinics. The project will include operational components (education, screening algorithms, telehealth and possibly onsite specialty providers) and infrastructure components (print/screen/app resources, telehealth equipment, clinic space with allies such Brookside Community Health Center and Southern Jamaica Plain Health Center).
The Oral Medicine group at BWH led by Dr. Piam Vacharotayangul, Dr. Brittany Klein (PGY-2) and Dr. Nathaniel Treister were awarded a significant fund through the United Against Racism initiative from the Mass General Brigham system. Aimed to address disparities in access to our oral medicine specialty from the underserved population, the fund will be used to systemically generate awareness of our practice to the general public and professional communities in Boston and its vicinities. By connecting to and establish a clinic in the local community health centers, the oral medicine group at BWH will be providing care to the people directly in the community and reducing the burden of commuting and waiting time to see our specialists. The team will foster trust by promoting a continuous commitment of the specialists within the underrepresented community, by providing education and outreach into the community on a regular basis, by demonstrating the outcomes that can be achieved, and by facilitating the referral to or access to specialized care clinics. The project will include operational components (education, screening algorithms, telehealth and possibly onsite specialty providers) and infrastructure components (print/screen/app resources, telehealth equipment, clinic space with allies such Brookside Community Health Center and Southern Jamaica Plain Health Center).